EXERCISE THERAPY
Definition
Exercises is physical activity that is planned, structured and repetitive for the
purpose of conditioning any part of the body. Exercise is utilized to improve health,
maintain fitness and is important as a means of physical rehabilitation.
There has been a gradually growing awareness among policy makers and health
care professionals about the great importance of appropriate exercise habits to
major public health outcomes. It has been known for decades that physical activity
prevents heart disease, rejuvenate our cells and aid in relaxation in most part but
data now suggest that, on average, physically active people outlive those who are
inactive and that regular physical activity helps to maintain the functional
independence of everyone especially older adults and to enhance the quality of life
for people of all ages. The basic elements of an exercise prescription for all ages
especially working adults are presented below.
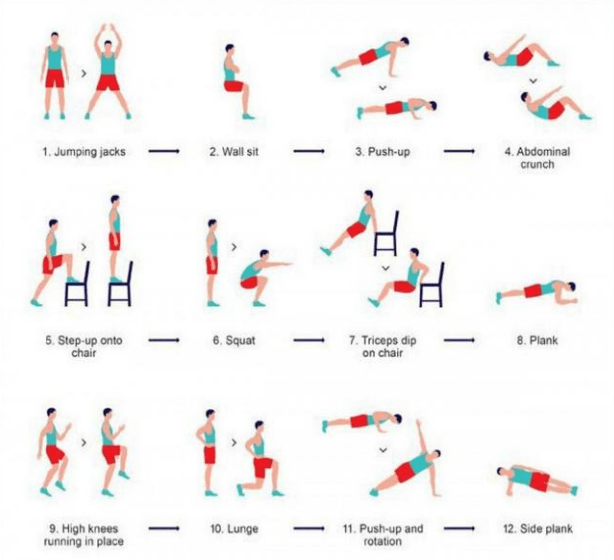
The 7-minutes exercise as illustrated above can be perform regularly every other
day, daily or twice a day depending on how often the best results can be achieve. If
these exercises are recommended by a physical therapy, then the resulting aptitude
can only be determined by follow up discussions.
Examples of balance enhancing activities include T’ai chi movements, standing
yoga or ballet postures, tandem standing and walking, standing on one leg,
stepping over objects, climbing up and down steps slowly, turning, and standing on
heels and toes.
Intensity is increased by decreasing the base of support (e.g., progressing from
standing on two feet while holding onto the back of a chair to standing on one foot
with no hand support); by decreasing other sensory input (e.g., closing eyes or
standing on a foam pillow); or by perturbing the center of mass (e.g., holding a
heavy object out to one side while maintaining balance, standing on one leg while
lifting the other leg out behind the body, or leaning forward as far as possible
without falling or moving the feet).
The rationale for the integration of a physical activity prescription into health care
for older adults is based on four essential concepts. First, there is a great similarity
between the physiologic changes that are attributable to disuse and those which
have been typically observed in aging populations, leading to the speculation that
the way in which people age may in fact be greatly affected by activity levels.
Second, chronic diseases increase with age, and exercise has now been shown to be
an independent risk factor and/or potential treatment for most of the major causes
of morbidity and mortality in Western societies, a potential that currently is vastly
underutilized. Third, traditional medical interventions do not typically address
disuse syndromes accompanying chronic disease, which may be responsible for
much of their associated disability. Exercise is particularly good at targeting
syndromes of disuse. Finally, many pathophysiological aberrations that are central
to a disease or its treatment are specifically addressed only by exercise, which
therefore deserves a place in the mainstream of medical care, not as an optional
adjunct. Therefore, understanding the effects of aging on exercise capacity and
how habitual physical activity can modify this relationship in the older adult,
including its specific utility in treating medical diseases, is critical for health care
practitioners of all disciplines.
Purpose
Exercise is useful in preventing or treating coronary heart disease, osteoporosis,
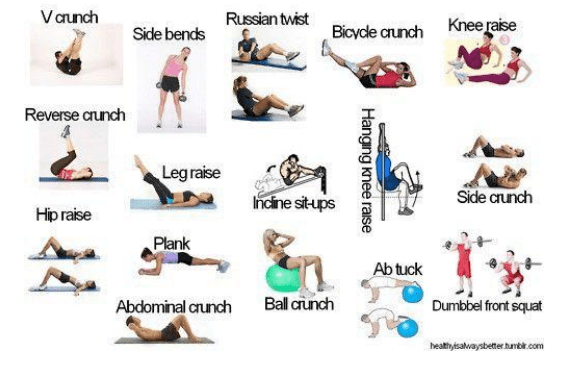
weakness, diabetes, obesity, and depression. Range of motion is one aspect of
exercise important for increasing or maintaining joint function. Strengthening
exercises provide appropriate resistance to the muscles to increase endurance and
strength. Cardiac rehabilitation exercises are developed and individualized to
improve the cardiovascular system for prevention and rehabilitation of cardiac
disorders and diseases. A well-balanced exercise program can improve general
health, build endurance, and slow many of the effects of aging. The benefits of
exercise not only improve physical health but also enhance emotional well-being.
Studies have shown that a consistent, guided exercise program benefits almost
everyone from Gulf War veterans coping with fatigue, distress, cognitive problems,
and mental health functioning to patients awaiting heart transplants. Exercise in
combination with a reduced-calorie diet is the safest and most effective method of
weight loss. The United States Department of Agriculture (USDA) food pyramid,
called MyPyramid, makes exercise as well as food recommendations to emphasize
the interconnectedness between exercise, diet, and health.
Precautions
Before beginning any exercise program, an evaluation by a physician is
recommended to rule out potential health risks. Once health and fitness level are
determined and any physical restrictions identified, the individual’s exercise
program should begin under the supervision of a health care or other trained
professional. This is particularly true when exercise is used as a form of
rehabilitation. If symptoms of dizziness, nausea, excessive shortness of breath, or
chest pain are present during exercise, the individual should stop the activity and
inform a physician about these symptoms before resuming activity. Exercise
equipment must be checked to determine if it can bear the weight of people of all
sizes and shapes. Individuals must be instructed in the proper use of exercise
equipment in order to prevent injury.
Other Forms of Exercises
Range of motion exercise
Range of motion exercise refers to activity aimed at improving movement of a
specific joint. This motion is influenced by several structures: configuration of
bone surfaces within the joint, joint capsule, ligaments, tendons, and muscles
acting on the joint. There are three types of range of motion exercises: passive,
active, and active assists. Passive range of motion is movement applied to a joint
solely by another person or persons or a passive motion machine. When passive
range of motion is applied, the joint of an individual receiving exercise is
completely relaxed while the outside force moves the body part, such as a leg or
arm, throughout the available range. Injury, surgery, or immobilization of a joint
may affect the normal joint range of motion. Active range of motion is movement
of a joint provided entirely by the individual performing the exercise. In this case,
there is no outside force aiding in the movement. Active assist range of motion is
described as a joint receiving partial assistance from an outside force. This range of
motion may result from the majority of motion applied by an exerciser or by the
person or persons assisting the individual. It also may be a half-and-half effort on
the joint from each source.
Strengthening exercise
Strengthening exercise increases muscle strength and mass, bone strength, and the
body’s metabolism. It can help attain and maintain proper weight and improve
body image and self-esteem. A certain level of muscle strength is needed to
perform daily activities such as walking, running, and climbing stairs.
Strengthening exercises increase muscle strength by putting more strain on a
muscle than it is normally accustomed to receiving. This increased load stimulates
the growth of proteins inside each muscle cell that allow the muscle as a whole to
contract. There is evidence indicating that strength training may be better than
aerobic exercise alone for improving self-esteem and body image. Weight training
allows one immediate feedback, through observation of progress in muscle growth
and improved muscle tone. Strengthening exercise can take the form of isometric,
isotonic and isokinetic strengthening.
Isometric exercise
During isometric exercises, muscles contract. However, there is no motion in the
affected joints. The muscle fibers maintain a constant length throughout the entire
contraction. The exercises usually are performed against an immovable surface or
object such as pressing one’s hand against a wall. The muscles of the arm are
contracting but the wall is not reacting or moving in response to the physical effort.
Isometric training is effective for developing total strength of a particular muscle
or group of muscles. It often is used for rehabilitation since the exact area of
muscle weakness can be isolated and strengthening can be administered at the
proper joint angle. This kind of training can provide a relatively quick and
convenient method for overloading and strengthening muscles without any special
equipment and with little chance of injury.
Isotonic exercise
Isotonic exercise differs from isometric exercise in that there is movement of a
joint during the muscle contraction. A classic example of an isotonic exercise is
weight training with dumbbells and barbells. As the weight is lifted throughout the
range of motion, the muscle shortens and lengthens. Calisthenics are also an
example of isotonic exercise. These would include chin-ups, push-ups, and sit-ups,
all of which use body weight as the resistance force.
Isokinetic exercise
Isokinetic exercise utilizes machines that control the speed of contraction within
the range of motion. Isokinetic exercise attempts to combine the best features of
both isometrics and weight training. It provides muscular overload at a constant
preset speed while a muscle mobilizes its force through the full range of motion.
For example, an isokinetic stationary bicycle set at 90 revolutions per minute
means that no matter how hard and fast the exerciser works, the isokinetic
properties of the bicycle will allow the exerciser to pedal only as fast as 90
revolutions per minute. Machines known as Cybex and Biodex provide isokinetic
results; they generally are used by physical therapists.
Cardiac rehabilitation
Exercise can be very helpful in prevention and rehabilitation of cardiac disorders
and disease. With an exercise program designed at a level considered safe for the
individual, people with symptoms of heart failure can substantially improve their
fitness levels. The greatest benefit occurs as muscles improve the efficiency of
their oxygen use, which reduces the need for the heart to pump as much blood.
While such exercise does not necessarily improve the condition of the heart itself,
the increased fitness level reduces the total workload of the heart. The related
increase in endurance also should translate into a generally more active lifestyle.
Endurance or aerobic routines, such as running, brisk walking, cycling, or
swimming, increase the strength and efficiency of the muscles of the heart.
Preparation
A physical examination by a physician is important to determine if strenuous
exercise is appropriate or detrimental for an individual, especially when the
exercise program is designed for rehabilitation. Before exercising, proper
stretching is important to prevent the possibility of soft tissue injury resulting from
tight muscles, tendons, ligaments, and other joint-related structures.
Aftercare
Proper cool down after exercise is important in reducing the occurrence of painful
muscle spasms. Proper cool down stretching also may decrease frequency and
intensity of muscle stiffness the day following any exercise program.
Risks
Improper warm up can lead to muscle strains. Overexertion without enough time
between exercise sessions to recuperate also can lead to muscle strains, resulting in
inactivity due to pain. Stress fractures also are a possibility if activities are
strenuous over long periods without proper rest. Although exercise is safe for the
majority of children and adults, there is still a need for further studies to identify
potential risks.
Normal results
Significant health benefits are obtained by including a moderate amount of
physical exercise in the form of an exercise prescription. This is much like a drug
prescription in that it also helps enhance the health of those who take it in the
proper dosage. Physical activity plays a positive role in preventing disease and
improving overall health status. People of all ages, both male and female, benefit
from regular physical activity. Regular exercise also provides significant
psychological benefits and improves quality of life.
Abnormal results
Exercise burnout may occur if an exercise program is not varied and adequate rest
periods are not taken between exercise sessions. Muscle, joint, and cardiac
disorders have been noted among people who exercise. However, they often have
had preexisting or underlying illnesses.
Key Terms
Aerobic
Exercise training that is geared to provide a sufficient cardiovascular
overload to stimulate increases in cardiac output.
Calisthenics
Exercise involving free movement without the aid of equipment.
Endurance
The time limit of a person’s ability to maintain either a specific force or
power involving muscular contractions.
Osteoporosis
A disorder characterized by loss of calcium in the bone, leading to thinning
of the bones. It occurs frequently in postmenopausal women.
Bibliography
Websites
- “Exercise and Physical Fitness.” MedlinePlus. February 25, 2009 [cited February 26, 2009]. http://www.nlm.nih.gov/medlineplus/exerciseandphysicalfitness.html.
- “Exercise for Children.” MedlinePlus. February 23, 2009 [cited February 26, 2009]. http://www.nlm.nih.gov/medlineplus/exerciseforchildren.html.
- “Exercise for Seniors.” MedlinePlus. February 18, 2009 [cited February 26, 2009]. http://www.nlm.nih.gov/medlineplus/exerciseforseniors.html.
Organizations
- American College of Sports Medicine. P. O. Box 1440, Indianapolis, IN 46206-1440. Telephone: (317) 637-9200. Fax: (317) 634-7817. http://www.acsm.org.
- American Medical Association. 515 N. State Street, Chicago, IL 60610. (800) 621-8335. http://www.ama-assn.org.
- American Physical Therapy Association. 1111 North Fairfax Street, Alexandria, VA 22314-1488. (800) 999-APTA (2782) or (703) 684-APTA (2782). TDD: (703) 683-6748. http://www.apta.org.
- National Athletic Trainers’ Association. 2952 Stemmons Freeway, Dallas, TX 75247-6916. (800) 879-6282 or (214) 637-6282. Fax: (214) 637-2206. http://www.nata.org
Retarding the aging process
In most physiologic systems, there is considerable evidence that the normal aging
processes do not result in significant impairment or dysfunction in the absence of
pathology, and under resting conditions. However, in response to a stress, the age-related reduction in physiologic reserves causes a loss of regulatory or homeostatic
balance. This process has been termed “homeostenosis” (a lessened capacity for
fine-tuning of the system). Thus, subtle changes in physical activity patterns over
the adult life span cause most people not engaged in athletic pursuits to lose a very
large proportion of their physical work capacity before they notice that something
is wrong or find that they have crossed a threshold of disability. The second
consequence of age-related changes in physiologic capacity is the increased
perception of effort associated with submaximal work. Thus a vicious cycle is set
up: “usual” aging leading to decreasing exercise capacity, resulting in an elevated
perception of effort, subsequently causing avoidance of activity, and finally
feeding back to exacerbation of the age-related declines secondary to disuse.
One of the major goals of gerontological research over the past several decades has
been to separate the true physiologic changes of aging from changes due to disease
or environmental factors, including disuse or underuse of body systems. Numerous
studies point out the superior physical condition of those who exercise regularly
compared to their more sedentary peers, even in the tenth decade of life. On the
other hand, research indicates that years of physiologic aging of diverse organ
systems and metabolic functions can be mimicked by short periods of enforced
inactivity, such as bed rest, wearing a cast, denervation, or absence of gravitational
forces. These two types of studies have led to a theory of disuse and aging which
suggests that aging as it is known in modern society is, in many ways, an exercise
deficiency syndrome. This implies that people may have far more control over the
rate and extent of the aging process than was previously thought.
Minimizing risk factors for chronic disease
Another way to integrate exercise into health care is to view it in light of its
potential to reduce risk factors for chronic diseases. The very large potential for exercise to act as a primary prevention tool is obvious from the kinds of risk factors and diseases listed. The major causes of morbidity and mortality (heart disease, stroke, diabetes, cancer, arthritis, functional dependency, hip fracture, and dementia) in the older population, are all more prevalent in individuals who are sedentary as compared to more active peers.
Adjunctive and primary treatment of chronic disease
There are various diseases in which exercise has a potentially valuable role
because of its ability to directly treat the pathophysiology of the disease. In some cases, exercise may provide benefits similar to those of medication or nutritional intervention; in others it may act through an entirely different pathway.
The chronic treatment of hypertension and coronary artery disease is clearly a case for management with both standard medical treatments and exercise. Exercise may prevent secondary cardiovascular events as well as minimize the need and risk of multiple drug use or high drug dosages in these conditions.
The benefits of exercise are often most dramatic in individuals in whom medical
treatment is already optimized and cannot be pushed further, or when the
pathophysiology of the disease itself is not amenable to change. For example, in
chronic obstructive pulmonary disease, once bronchospasm has been relieved and
oxygen has been supplemented, exercise tolerance may still be very limited due to
peripheral skeletal muscle atrophy and inability to effectively extract oxygen and
utilize it for aerobic work as a result of years of disuse, poor nutrition, and other
factors. However, such peripheral abnormalities can be directly and effectively
targeted and treated with progressive endurance training protocols, which have
been shown to significantly improve exercise tolerance, functional status, and
quality of life in such patients.
How to minimize risk factor for chronic diseases?
Minimizing the risk factors for chronic diseases involves adopting a healthy lifestyle and making informed choices. Here are some key strategies:
- Quit Smoking: Smoking is a major risk factor for many chronic diseases, including heart disease, cancer, and chronic obstructive pulmonary disease (COPD). Quitting smoking can significantly reduce these risks.
- Eat Healthy: A balanced diet rich in fruits, vegetables, whole grains, lean proteins, and low-fat dairy products can help prevent and manage chronic diseases like heart disease, diabetes, and cancer. Limiting added sugars, saturated fats, and sodium is also important.
- Regular Physical Activity: Engaging in regular physical activity, such as brisk walking, gardening, or other moderate-intensity exercises, for at least 150 minutes a week can help prevent and manage chronic diseases.
- Limit Alcohol Consumption: Excessive alcohol consumption can lead to high blood pressure, various cancers, heart disease, stroke, and liver disease. Reducing alcohol intake can lower these health risks.
- Get Regular Screenings: Regular checkups and screenings can help detect chronic diseases early and manage them effectively. This includes cancer screenings, diabetes testing, and dental check-ups.
- Maintain a Healthy Weight: Achieving and maintaining a healthy weight through diet and exercise can reduce the risk of chronic diseases such as diabetes, heart disease, and certain cancers.
- Manage Stress: Chronic stress can contribute to the development of chronic diseases. Practicing stress management techniques like meditation, yoga, and deep breathing can help reduce stress levels.
- Get Enough Sleep: Adequate sleep is essential for overall health. Adults should aim for at least 7 hours of sleep per night to reduce the risk of chronic diseases.
- Know Your Family History: Understanding your family history of chronic diseases can help you take preventive measures and catch potential issues early.
By incorporating these healthy habits into your daily routine, you can significantly reduce your risk of developing chronic diseases and improve your overall well-being.
What are the major causes of morbidity and mortality (heart disease, stroke, diabetes, cancer, arthritis, functional dependency, hip fracture, and dementia) in the older population?
The major causes of morbidity and mortality in the older population include a range of chronic diseases and conditions. Here are some of the key factors:
- Heart Disease: Leading cause of death among older adults, including conditions like coronary artery disease, heart failure, and arrhythmias.
- Cancer: Various types of cancer, such as lung, colorectal, breast, and prostate cancer, are significant causes of mortality.
- Stroke: Also known as cerebrovascular disease, stroke is a major cause of death and disability in older adults.
- Diabetes: Both type 1 and type 2 diabetes can lead to serious complications, including cardiovascular disease, kidney failure, and neuropathy.
- Chronic Lower Respiratory Diseases: Conditions like chronic obstructive pulmonary disease (COPD), emphysema, and chronic bronchitis are common.
- Arthritis: Osteoarthritis and rheumatoid arthritis cause significant morbidity due to pain and reduced mobility.
- Functional Dependency: Loss of independence due to physical or cognitive decline, often requiring long-term care.
- Hip Fracture: Common in older adults due to falls, leading to significant morbidity and mortality.
- Dementia: Including Alzheimer’s disease, dementia leads to cognitive decline and is a major cause of disability and dependency.
These conditions highlight the importance of preventive measures, early detection, and effective management to improve the quality of life for older adults.
How are the prevention, treatments and cures of these diseases?
Preventing, treating, and managing chronic diseases involves a combination of lifestyle changes, medical interventions, and ongoing care. Here’s a detailed look at each:
Heart Disease
Prevention:
- Healthy Diet: Eat plenty of fruits, vegetables, whole grains, and lean proteins. Limit saturated fats, trans fats, and sodium.
- Regular Exercise: Engage in at least 150 minutes of moderate-intensity exercise per week.
- Quit Smoking: Smoking cessation significantly reduces heart disease risk.
- Manage Stress: Practice stress-reducing techniques like meditation and yoga.
Treatments:
- Medications: Include statins, beta-blockers, and ACE inhibitors to manage cholesterol, blood pressure, and heart function.
- Surgical Procedures: Angioplasty, stent placement, and coronary artery bypass grafting (CABG) for severe cases.
Cures:
- Lifestyle Changes: While not a cure, significant lifestyle changes can manage and sometimes reverse heart disease.
Stroke
Prevention:
- Control Blood Pressure: Maintain healthy blood pressure levels.
- Healthy Diet: Similar to heart disease prevention, focus on a balanced diet.
- Exercise: Regular physical activity helps maintain healthy blood vessels.
- Avoid Smoking: Smoking cessation is crucial.
Treatments:
- Medications: Thrombolytics like tPA for ischemic stroke, anticoagulants, and antiplatelet drugs.
- Surgical Procedures: Carotid endarterectomy, aneurysm clipping, and thrombectomy.
- Rehabilitation: Physical, occupational, and speech therapy to recover lost functions.
Cures:
- Immediate Treatment: Quick medical intervention can significantly reduce long-term damage.
Diabetes
Prevention:
- Healthy Diet: Focus on low-sugar, high-fiber foods.
- Regular Exercise: Helps maintain healthy blood sugar levels.
- Weight Management: Maintain a healthy weight to reduce risk.
Treatments:
- Medications: Insulin, metformin, and other glucose-lowering drugs.
- Lifestyle Changes: Diet and exercise are crucial components.
Cures:
- Remission: While not a cure, some people achieve remission through significant lifestyle changes and medical interventions.
Cancer
Prevention:
- Avoid Tobacco: Smoking cessation reduces the risk of many cancers.
- Healthy Diet: Eat a diet rich in fruits, vegetables, and whole grains.
- Regular Screenings: Early detection through screenings like mammograms and colonoscopies.
- Vaccinations: HPV and hepatitis B vaccines can prevent certain cancers.
Treatments:
- Surgery: Removal of tumors.
- Radiation Therapy: Uses high-energy rays to kill cancer cells.
- Chemotherapy: Uses drugs to kill cancer cells.
- Immunotherapy: Boosts the body’s immune system to fight cancer.
Cures:
- Early Detection and Treatment: Some cancers can be cured if detected early and treated effectively.
Arthritis
Prevention:
- Maintain Healthy Weight: Reduces stress on joints.
- Regular Exercise: Strengthens muscles around joints.
- Healthy Diet: Anti-inflammatory foods can help.
Treatments:
- Medications: NSAIDs, corticosteroids, and DMARDs.
- Physical Therapy: Improves joint function and reduces pain.
- Surgery: Joint replacement or repair in severe cases.
Cures:
- Management: While not curable, symptoms can be managed effectively.
Functional Dependency
Prevention:
- Regular Exercise: Maintains physical function.
- Healthy Diet: Supports overall health.
- Social Engagement: Reduces the risk of cognitive decline.
Treatments:
- Rehabilitation Services: Physical and occupational therapy.
- Assistive Devices: Tools to aid daily living.
Cures:
- Management: Focuses on maintaining independence and quality of life.
Hip Fracture
Prevention:
- Fall Prevention: Home safety measures and balance exercises.
- Bone Health: Adequate calcium and vitamin D intake.
Treatments:
- Surgery: Internal repair, partial or total hip replacement.
- Rehabilitation: Physical therapy to regain mobility.
Cures:
- Surgical Repair: Effective treatment for most hip fractures.
Dementia
Prevention:
- Healthy Lifestyle: Diet, exercise, and mental stimulation.
- Manage Chronic Conditions: Control blood pressure, diabetes, and cholesterol.
Treatments:
- Medications: Cholinesterase inhibitors and memantine.
- Therapies: Cognitive stimulation and occupational therapy.
Cures:
- Management: Focuses on slowing progression and improving quality of life.
These strategies highlight the importance of a proactive approach to health, combining lifestyle changes with medical interventions to prevent, treat, and manage chronic diseases.
References:
The exercise prescription
This section will outline the elements of a prescription designed to stimulate robust
adaptation within the major physiologic domains that can be modified by exercise:
strength, cardiovascular endurance, flexibility, and balance, as recommended by
the American College of Sports Medicine and endorsed by most major medical
consensus groups. These elements are discussed separately, because in most cases
exercise training is quite specific in its effects, and little crossover will be seen. For
example, balance training will not increase one’s aerobic capacity or strength.
Resistance training is unique in this regard; it has been shown to benefit all of these
domains to some extent, with its most powerful effect in the realms of muscle
strength and endurance.
Progressive resistance training. Progressive resistance training (PRT) is the
process of challenging the skeletal muscle with an unaccustomed stimulus, or load,
such that neural and muscle tissue adaptations take place, leading ultimately to
increased strength and muscle mass. In this kind of exercise, the muscle is
contracted slowly just a few times in each session against a relatively heavy load.
Any muscle may be trained in this way, although usually six to twelve major
muscle groups with clinical relevance are trained, for a balanced and functional
outcome. The most important element of the PRT prescription is the intensity of
the load used. It is evident from many years of research and clinical practice that
muscle strength and size are increased significantly only when the muscle is loaded
at a moderate or high intensity (60–100 percent of maximum).
The benefits of PRT are both metabolic and functional. It improves sensitivity to
insulin and may therefore be important in both the prevention and the treatment of
diabetes. It also increases bone formation and density, and has a role in the
prevention and treatment of osteoporosis. It significantly improves muscle strength
and is associated with muscle hypertrophy, and is therefore useful whenever
muscle weakness or atrophy contributes to disease or dysfunction. Such disease or
dysfunction includes falls, frailty, chronic heart failure, chronic lung disease,
Parkinson’s disease, neuromuscular disease, chronic renal failure, arthritis, and
other chronic conditions associated with decreased activity levels and impaired
mobility. In addition, PRT has marked psychological benefits, having been shown
to improve major depression as well as insomnia, self-efficacy, and emotional
well-being in older adults.
The potential risks of PRT are primarily musculoskeletal injury and rarely
cardiovascular events (ischemia, arhythnias, hypertension). Musculoskeletal injury
is almost entirely preventable with attention to the following points:
- Adherence to proper form.
- Isolation of the targeted muscle group.
- Slow velocity of lifting.
- Limitation of range of motion to the pain-free arc of movement.
- Avoidance of use of momentum and ballistic movements to complete a lift.
- Use of machines or chairs with good back support.
- Observation of rest periods between sets and rest days between sessions.
- Cardiovascular endurance training.
Cardiovascular endurance training refers to exercise in which large muscle groups contract many times (thousands of times at a single session) against little or no resistance other than that imposed by gravity.
The purpose of this type of training is to increase the maximal amount of aerobic
work that can be carried out, as well as to decrease the physiologic response and
perceived difficulty of submaximal aerobic workloads. Extensive adaptations in
the cardiopulmonary system, peripheral skeletal muscle, circulation, and
metabolism are responsible for these changes in exercise capacity and tolerance.
Many different kinds of exercise fall into this category, including walking and its
derivatives (hiking, running, dancing, stair climbing), as well as biking, swimming,
ball sports, etc.
The key distinguishing features between activities that are
primarily aerobic versus resistive in nature.
There may be some overlap if aerobic activities are altered to increase the loading to
muscle, as in resisted stationary cycling or stair-climbing machines. However, such
activities are still primarily aerobic in nature, because they do not cause fatigue
within a very few contractions, as PRT does, and therefore do not result in the
kinds of adaptations in the nervous system and muscle that lead to marked strength
gain and hypertrophy.
Overall, walking and its derivations surface as the most widely studied, feasible,
safe, accessible, and economical mode of aerobic training for men and women of
most ages and states of health. They do not require special equipment or locations,
and do not need to be taught or supervised (except in the cognitively impaired,
very frail, or medically unstable individual). Walking bears a natural relationship
to ordinary activities of daily living, making it easier to integrate into lifestyle and
functional tasks than any other mode of exercise. Therefore, it may be more likely
to translate into improved functional independence and mobility than other modes
of exercise.
The intensity of aerobic exercise refers to the amount of oxygen consumed,
or energy expended, per minute while performing the activity, which will vary
from about 5 kcal/minute for light activities, to 7.5 kcal/minute for moderate
activities, to 10–12 kcal/minute for very heavy activities. Energy expenditure
increases with increasing body weight for weight-bearing aerobic activities, as well
as with inclusion of larger muscle mass, and increased work (force x distance) and
power output (work/time) demands of the activity. Therefore, the most intensive
activities are those which involve the muscles of the arms, legs, and trunk
simultaneously, necessitate moving the full body weight through space, and are
done at a rapid pace (e.g.. cross-country skiing). Adding extra loading to the body
weight (back-pack, weight belt, wrist weights) increases the force needed to move
the body part through space, and therefore increases the aerobic intensity of the
work performed. The rise in heart rate is directly proportional, in normal
individuals, to the increasing oxygen consumption or aerobic workload. Thus,
monitoring heart rate has traditionally been a primary means of both prescribing
appropriate intensity levels and following training adaptations when direct
measurements of oxygen consumption are not available.
The relative heart rate reserve (HRR) is the most useful estimate of intensity based on heart rate. T raining intensity is normally recommended at approximately 60 to 70 percent of the HRR.
It is calculated as is shown below.
HRR = (Maximal heart rate – resting heart rate) + resting heart rate 60–70% HRR
=.6–.7(Max HR -resting HR) + resting HR
Therefore, a more easily obtainable and reliable estimate of aerobic intensity is to
prescribe a level of “somewhat hard,” or 12 to 14 on the Borg scale, which runs
from 6 to 20. At this level, the exerciser should note increased pulse and
respiratory rate, but still be able to talk. All of the major benefits of aerobic
exercise (increased cardiovascular fitness, decreased mortality, decreased
incidence of chronic diseases, improved insulin sensitivity, blood pressure, and
cholesterol, for example) are attainable with this moderately intense level of
aerobic training. As is the case with all other forms of exercise, in order to
maintain the same relative training intensity over time, the absolute training load
must be increased as fitness improves. The workloads should progress on the basis
of ratings of effort at each training session. Once the perceived exertion slips
below, the intensity of the regimen should be increased to maintain the
physiologic stimulus for optimal rates of adaptation. As with PRT, the most
common error in aerobic training is failure to progress, which results in an early
plateau in cardiovascular and metabolic improvement.
Cardiovascular protection and risk factor reduction appear to require twenty to
thirty minutes three days per week, as does improvement in aerobic capacity.
Epidemiological studies of mortality, cardiovascular disease, diabetes and
functional independence suggest that walking about one mile per day (presumably
about twenty minutes at average pace) or expending about 2000 kcal/week in
physical activities is protective, again pointing to the moderate levels that are
needed for major health outcomes. It has been shown that exercise does not need to
be carried out in a single session to provide training effects, and may be broken up
into periods of ten minutes at a time.
The risk of sudden death during
physical activity appears to be limited primarily to those who do not exercise on a
regular basis (at least one hour per week), which is another reason for advocating
regular, moderate periods of exercise rather than periodic high-volume training.
The benefits of aerobic exercise have been extensively studied since the 1960s.
They include a broad range of physiological adaptations that are in general opposite to the effects of aging on most body systems, as well as major health-related clinical outcomes. The health conditions that are responsive to aerobic exercise include most of those of
concern to older adults: osteoporosis, heart disease, stroke, breast cancer, diabetes,
obesity, hypertension, arthritis, chronic lung disease, depression, and insomnia.
These physiological and clinical benefits form the basis for the inclusion of aerobic
exercise as an essential component of the overall physical activity prescription for
healthy aging.
Flexibility training. Flexibility training includes movements or positions designed
to increase range of motion across joints. Such range of motion is determined by
both soft tissue factors (muscle strength, muscle and ligament length, scarring from
surgery or trauma, joint and bursa fluid, synovial tissue thickness and inflammation,
ligament laxity, tissue elasticity, degenerative changes of cartilage, temperature of
tissues) and bony structure (deformities, arthritic and degenerative changes in bone,
surgical devices). Obviously, only some of these abnormalities are amenable to
exercise intervention, and these will be discussed below. In general, the effect of
stretching the soft tissues around a joint slowly and consistently over time is to
increase the pain-free range of motion for that joint.
Flexibility may be enhanced without the use of any specialized equipment. It is
often helpful, however, to have a thin mat available for postures that are best done
while stretched out on the floor.
The most effective technique for increasing flexibility is to extend a body part as
fully as possible without pain, then hold this fully extended position for twenty to
thirty seconds. The key requirement is to complete the movement slowly (without
any bouncing or ballistic movements). Such bouncing does not increase efficacy
and range of motion, but instead may cause muscle contraction that limits the
range achievable. A technique known as proprioceptive neural facilitation (PNF)
will maximize the stretching effectiveness. The technique is as follows. Once the
body part has been stretched as far as possible, the muscle groups around the joint
should then be completely relaxed, while maintaining the stretch. Next, an attempt
is made to stretch a little further, which is usually possible. This final position is
then held for about twenty to thirty seconds before returning to the initial position.
PNF serves to counteract the involuntary resistance to overextension of a joint
caused by a feedback loop of receptors within the muscle tissue that are activated
by mechanical stretch.
Flexibility exercise is part of many other forms of exercise, such as ballet and
modern dance, yoga, t’ai chi, and resistance training, because in all of these
pursuits the muscle groups are slowly extended to their full range and held before
relaxing, just as in PNF. It is not recommended to force a stretch beyond the point
of pain, as this may result in injury to soft tissue structures and ultimately worsen
function. As with all forms of exercise, as the range of motion increases over time,
it is appropriate and necessary to extend the distance the joint is moved so that
progress is maintained.
The physiologic benefit of flexibility exercise is increased range of motion across
joints. There is some evidence that range of motion is related to functional
independence in activities of daily living, posture, balance, and gait characteristics
in older adults, as well as to pain and disability and quality of life in arthritis.
Flexibility training itself does not result in improved strength or endurance, or
marked improvements in balance. Therefore, it is best conceived of as an accessory
to other forms of exercise that contributes to overall exercise and functional
capacity. To the extent that pain, fear of falling, mobility, and function are
improved, quality of life may improve as well. There is a need for much better
quantitative research on effective doses and long-term benefits of this mode of
exercise in the elderly.
Balance training. Any activity that increases one’s ability to maintain balance in
the face of stressors may be considered a balance-enhancing activity. Stressors
include decreased base of support; perturbation of the ground support; decrease in
proprioception, vision, or vestibular system input; increased compliance of the
support surface; or movement of the center of mass of the body.
Balance enhancing activities impact on the central nervous system control of balance and
coordination of movement, and/or augment the peripheral neuromuscular system
response to signals that balance is threatened.
Intensity in balance training refers to the degree of difficulty of the postures,
movements, or routines practiced. The appropriate level of difficulty or “intensity”
for any balance-enhancing exercise is the highest level that can be tolerated
without inducing a fall or near-fall. Progression in intensity is the key to
improvement, as in other exercise domains, but mastery of the previous level
before progression must be adhered to for safety.
Balance training has been shown to result in improved balance performance,
decreased fear of falling, decreased incidence of falls, and increased ability to
participate in activities of daily living that may have been limited by gait and
balance difficulties. It is expected, although not proven, that such changes
ultimately lead to improvements in functional independence, reduced hip fractures
and other serious injuries and improved overall quality of life.
Summary of benefits
Physiologic aging, retirement, societal expectations, accumulated diseases, and
medication and nutritional effects conspire to produce deficits in strength, balance,
aerobic capacity, and flexibility in older adults. Fortunately, there is increasing
evidence for the reversibility of many of these deficits with a targeted exercise
prescription. There is still work to be done in refining the prescription, particularly
in terms of the amount of flexibility and balance training needed for optimal
efficacy. In addition, there is a need for well-controlled, long-term studies on
clinically important outcomes, such as treatment of cardiovascular disease and
stroke, prevention and treatment of hip fracture, prevention of diabetic
complications, reduction in nursing home admission rates, and moderation of
disability from arthritis. An “active lifestyle” may be the most desirable public
health approach to the maintenance of function and the prevention of disease in
healthy persons. However, it is likely that the use of exercise to treat preexisting
diseases and geriatric syndromes will always need to incorporate elements of a
traditional “exercise prescription,” as well as behavioral approaches, to more fully
integrate appropriate physical activity into daily life.
what is Sarcopenia?
Sarcopenia is the age-related progressive loss of muscle mass, strength, and function. It primarily affects older adults and can significantly impact their quality of life by reducing their ability to perform daily tasks. The term comes from the Greek words “sarx” (flesh) and “penia” (poverty), reflecting to the loss of muscle tissue.
Causes
- Aging: Natural aging processes lead to a decrease in muscle mass and strength.
- Physical Inactivity: Lack of regular exercise can accelerate muscle loss.
- Hormonal Changes: Changes in hormones like testosterone and insulin-like growth factor (IGF-1) can affect muscle fibers.
- Nutrition: Inadequate protein intake and poor nutrition can contribute to muscle loss.
Symptoms
- Muscle Weakness: The most common symptom, leading to difficulty in performing daily activities.
- Reduced Stamina: Decreased ability to carry out physical activities.
- Balance Issues: Increased risk of falls and fractures due to weakened muscles.
Prevention and Treatment
- Exercise: Regular physical activity, especially resistance training, can help maintain muscle mass and strength.
- Nutrition: Adequate protein intake and a balanced diet are crucial.
- Hormone Replacement Therapy: In some cases, hormone therapy may be considered, though it comes with risks.
Sarcopenia is a significant factor that increases in frailty, falls, and fractures among the elderly. Addressing it through lifestyle changes and medical interventions can greatly improve quality of life.
Valerie Njee
Related topics: Exercise; Balance and Mobility; Balance, Sense of; Frailty; Heart Disease; Life Expectancy; Periodic Health Examination; Sarcopenia.
BIBLIOGRAPHY
American College of Sports Medicine. “The Recommended Quantity and Quality of Exercise for
Developing and Maintaining Cardiopulmonary and Muscular Fitness in Healthy Adults.”
Medicine and Science in Sports and Exercise 22 (1990): 265–274.
American College of Sports Medicine. Guidelines for Exercise Testing and Prescription.
Philadelphia: Williams & Wilkins, 1995.
Blair, S. N.; Kohl, H.; Barlow, C.; et al. “Changes in Physical Fitness and All-Cause Mortality:
A Prospective Study of Healthy and Unhealthy Men.” Journal of the American Medical
Association 273 (1995): 1093–1098.
Bortz, W. M. “Redefining Human Aging.” Journal of the American Geriatrics Society 37 (1989):
1092–1096.
Drinkwater, B.; Grimson, S.; Cullen-Raab, D.; et al. “ACSM Position Stand on Osteoporosis and
Exercise.” Medicine and Science in Sports and Exercise 27 (1995): i–vii.
Fiatarone Singh, M. Exercise, Nutrition and the Older Woman: Wellness for Women over Fifty
Boca Raton, Fla.: CRC Press, 2000.
Helmrich, S.; Ragland, D.; and Paffenbarger, R. “Prevention of Non-Insulin-Dependent Diabetes
Mellitus with Physical Activity.” Medicine and Science in Sports and Exercise 26 (1994): 824–
830.
Lee, I.-M.; Paffenbarger, R. S.; and Hennekens, C. H. “Physical Activity, Physical Fitness and
Longevity.” Aging Clinical and Experimental Research 9 (1997): 2–11.
Mazzeo, R.; Cavanaugh, P.; Evans, W.; et al. “Exercise and Physical Activity for Older Adults.”
Medicine and Science in Sports and Exercise 30 (1998): 992–1008.
Miller, M.; Rejeski, W.; Reboussin, B.; et al. “Physical Activity, Functional Limitations, and
Disability in Older Adults.” Journal of the American Geriatrics Society 48 (2000): 1264–1272.
National Institute of Health, Center for Disease Prevention. “Physical Activity and
Cardiovascular Health.” Journal of the American Medical Association 276 (1996): 241–246.
Pate, R. R.; Pratt, M.; Blair, S. N.; et al. “Physical Activity and Public Health: A
Recommendation From the Centers for Disease Control and Prevention and the American
College of Sports Medicine.” Journal of the American Medical Association 273 (1995): 402–407.
Province, M.; Hadley, E.; Hornbrook, M.; et al. “The Effects of Exercise on Falls in Elderly
Patients.” Journal of the American Medical Association 273 (1995): 1341–1347.
U.S. Department of Health and Human Services. Physical Activity and Health: A Report of the
Surgeon General. Atlanta, Ga.: U.S. Dept. of Health and Human Services, Centers for Disease
Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion,1996.
